A 45 yr old female with fever, vomiting
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 45 yr old female house wife came to casuality with cheif complaints of fever since 4 days, vomitings since 4 days
Patient was apparently asymptomatic 4 days back the developed fever low grade , intermittent type
Relieved on medication
Associated with chills and rigor , no diurnal variation
Vomitings sonce 4 days non projectile, non bilious , not associated with pain abdomen
Past history
No h/ o DM, HTN, asthma , TB, epilepsy
Personal history
She is married
Mixed diet, normal appetite
Adequate sleep, bowel bladder movements are regular, normalno addictions
Family history - not significant
General examination
Pt c/c/c
Vitals-
Temperature- 100 F
BP- 110/80mmhg
Pr- 80 bpm
Systemic examination
Cvs- s1, s2 heard
Rs- BAE+, NVBS
P/A- soft, non tender
CNS- intact
Provisional diagnosis:
Dengue fever( NS1 POSITIVE)
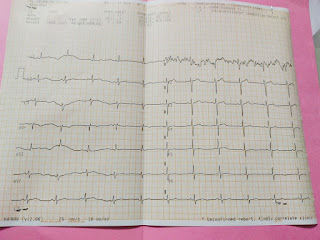
Ecg
Chest x ray
Investigations
Hemogram at time of admission
Hb- 16.9
Tlc-2,500
Rbc-5.20
Plt-55,000
Serum urea- 21
Serum creatinine-0.9
Na+ 137
K+ 4.8
Cl- 99
LFT
TB- 0.39
DB- 0.16
AST- 108
ALT- 80
ALP- 169
TP- 5.6
ALB- 3.5
A/G- 1.72
RBS-205
STOOL FOR OCCULT BLOOD - POSITIVE
Hemogram 28/9/21 mrng
Hb- 13.7
Tlc- 4,300
Rbc-5.10
Plt- 65,000
Treatment given
Day 1
1) IVF ( NS, RL)
2) INJ PAN 40 mg IV/ OD
3) INJ ZOFER 4 mg IV/ BD
4)TAB PCM 650 mg PO/ SOS
5) INJ BUSCOPAN 1 amp IV/ SOS
6) watch for bleeding manifestations
7) Vitals monitoring every 6 th hrly
Day 2
Treatment given
1) IVF ( NS, RL)
2) INJ PAN 40 mg IV/ OD
3) INJ ZOFER 4 mg IV/ BD
4)TAB PCM 650 mg PO/ SOS
5) INJ BUSCOPAN 1 amp IV/ SOS
6) watch for bleeding manifestations
7) Vitals monitoring every 6 th hrly
Discharge summary:
Date- 29/09/21
Ward- gm
Unit- 1
Treating faculty:
Dr valli( intern)
Dr akshitha( intern)
Dr tejaswini( intern)
Dr roshna( intern)
Dr kusuma( intern)
Dr raveen( pgy1)
Dr k vaishnavi( pgy3)
Dr nikhitha( pgy3)
Dr hareen( sr)
Dr arjun( ap)
Dr rakesh biswas( hod)
Diagnosis:
Dengue fever( NS1 POSITIVE)
Clinical history, findings:
A 45 yr old female house wife came to casuality with cheif complaints of fever since 4 days, vomitings since 4 days
Patient was apparently asymptomatic 4 days back the developed fever low grade , intermittent type
Relieved on medication
Associated with chills and rigor , no diurnal variation
Vomitings sonce 4 days non projectile, non bilious , not associated with pain abdomen
Past history
No h/ o DM, HTN, asthma , TB, epilepsy
Personal history
She is married
Mixed diet, normal appetite
Adequate sleep, bowel bladder movements are regular, normalno addictions
Family history - not significant
General examination
Pt c/c/c
Vitals-
Temperature- 100 F
BP- 110/80mmhg
Pr- 80 bpm
Systemic examination
Cvs- s1, s2 heard
Rs- BAE+, NVBS
P/A- soft, non tender
CNS- intact
Investigations:
Chest x ray normal
Usg abdomen- grade1 fatty liver
Ecg - within normal limits
Treatment given:
Day 1
1) IVF ( NS, RL)
2) INJ PAN 40 mg IV/ OD
3) INJ ZOFER 4 mg IV/ BD
4)TAB PCM 650 mg PO/ SOS
5) INJ BUSCOPAN 1 amp IV/ SOS
6) watch for bleeding manifestations
7) Vitals monitoring every 6 th hrly
Day 2
1) IVF ( NS, RL)
2) INJ PAN 40 mg IV/ OD
3) INJ ZOFER 4 mg IV/ BD
4)TAB PCM 650 mg PO/ SOS
5) INJ BUSCOPAN 1 amp IV/ SOS
6) watch for bleeding manifestations
7) Vitals monitoring every 6 th hrly
Advice at discharge:
1) plenty of oral fluids
2) TAB . PANTOP 40 mg PO/ OD before break fast for 5 days
3)TAB . LEVICITRIZENE 10 mg PO/ HS for 5 days
4) TAB. MVT PO/ OD at 2pm
for 10 days




Comments
Post a Comment