This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
UNIT 1 ADMISSION :
Unit 1 admission :
Icu bed 3
A 53 year old male ,cycle repairer by occupation came to the opd with chief complaints shortness of breath since 45 mins
C/O pedal edema in left leg upto ankle since 15 days
C/O cough with blood tinged sputum since 15 days
Pt was apparently asymptomatic 1 month back when he had 6 - 7 episodes of vomitings , associated with pain abdomen and loose stools (4- 5 episodes /day )for which he was admitted in government hospital and was given I .v fluids with loose stools persistent but decreased frequency since then ,not associated with fever .
He then developed pedal edema associated with cough with sputum which is blood tinged scanty,not associated with chest pain , associated with intermittent SOB which decreased on treatment
Pt continued to smoke 1 pack cigarrete /day ,after smoking he suddenly developed SOB at rest for 45 mins associated with profuse sweating and was brought here
H/O decreased urine output since 1 month
History of chest pain 6 months back diagnosed as MI ,PTCA ( ? 2 DES ) not on regular follow up
In the month of April, patient had sudden onset sob , profuse sweating, and retrosternal pain for which he was taken to a hospital near nalgonda where they thrombolysed him with streptokinase , after which they send him to Hyderabad where he underwent ptca , where a drug eluding stent to LCX was placed,
He was started on dual anti platelets and statin, after which he didn't have symptoms of sob or pedal edema till 15 days prior to admission,
He underwent ptca approximately one day after he was thrombolysed
Chronic smoker since 40 -45 days
,1 pack cigarette /day
Chronic alcoholic since 30 yrs,stopped 6 months back
H/O right lower limb below knee amputation 3p yrs back (RTA)
Pt is conscious, coherent,cooperative
No signs of pallor,icterus,cyanosis,clubbing, lymphadenopathy,edema
Vitals :
Temp - Afebrile
Pr: 130 /min ,low volume
Bp : not recordable
Spo2 : 56 %
Grbs : 123 mg/dl
CVS : S1,S2 heard
RS : dyspnea present
Breath sounds decreased in rt side
Coarse crepitus in left ISA ,IMA ,IAA
P/A :
distended abdomen
,Shifting dullness present
Bowel sounds heard
Diagnosis:
A -cardiogenic shock secondary to HFrEF with TYPE 1 Respiratory failure secondary to moderate hemorrhagic pleural effusion secondary to ?consolidation ,?malignancy with K/C/O CAD S/P PTCA ( 2 drug eluting stents )2 LCX 6 months back, AKI(pre renal ) with ischemic hepatitis
Patient was intubated at 2am and extubated at 1 pm today
INVESTIGATIONS :
Chest xray:
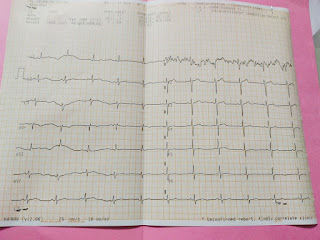
ECG AT THE TIME OF ADMISSION:
ECG AFTER SHIFTING TO ICU:
Hb - 13.9
TLC - 17700
RBC - 4.91
PLT - 1.16
CUE
ALB:+
EPITHELIAL CELLS:2-3 cells
PUS CELLS- 3-4 cells
urea - 70 mg/dl
Creat - 1.3
Na - 127
K - 5.1
Cl - 92
Tb- 2.93
Db - 0.95
AST - 83
ALT - 44
ALP - 213
TP - 5.9
albumin - 2.3
A/G ration - 0.65
Rat - negative
Serology - negative
BT: 2 min
CT:4 min 30 sec
PT- 18sec
INR- 1.2
Ldh - 790.7 IU/L
PLEURAL FLUID
SUGAR - 40 mg/dl
Ldh - 1153
PLEURAL FLUID CYTOLOGY
color- slightly reddish, appearence- hazy
TLC- 15,200 cells/cu.mm
N- 20
L-80
SERUM LIPASE-39
PLEURAL FLUID CYTOLOGY
cyto smear shows acute inflammatory exudates with neutrophils, occasional lymphocytes, reactive mesoepithelial cells over pale proteinecious background
Hb- 0.06
Pcv-0.2
USG CHEST
USG ABDOMEN
ENDOTRACHEAL TUBE AFTER EXTUBATION
CHEST XRAY AFTER PLEURAL TAP
CHEST XRAY ON 8/9/21
On 8/9/21
HB- 11.6
TLC-18,700
PLT- 1.50
RBC-4.08
LFT:
TB- 4.87
DB-2.82
AST- 68
ALT-41
ALP-183
TP-4.4
ALB-1.8
RFT
UREA-141
CREATININE-1.9
Ca2+: 8.2
Na+: 129
K+: 4.5
Cl- : 98
On 9/9/21
HB-11.2
TLC-17,700
RBC-3.98
PLT-1.46
RFT
UREA- 146
CREATININE-1.7
URICACID-7.7
Ca2+: 9.9
Na+:131
K+:3.7
Cl-: 96
On 10/9/21
HB-10.6
TLC-18,500
RBC-3.79
PLT-1.50
PT-16sec
INR-1.11
RFT
UREA- 152
CREATININE-2
URICACID-7.2
Ca2+: 8.3
Na+:130
K+:4.9
Cl-: 95
On 11/9/21
HB-10.9
TLC-20,500
RBC-3.89
PLT-1.54
LFT:
TB- 5.67
DB-2.89
AST- 48
ALT-30
ALP-185
TP-5.1
ALB-2
RFT
UREA-146
CREATININE-2
Ca2+: 9.1
Na+: 131
K+: 4.3
Cl- : 96
PT: 18 sec
INR- 1.3
Soap notes :
Day 2 of admission :
S - SOB with sats 56% at the time of admission
Intubated at 2 am yesterday and extubated at 1 pm
Pleural tap done
Patient subjectively feeling better with no fresh complaints
O -Temp : Afebrile
Bp : 90/60
Pr : 110 bpm
Spo2: 92
CVS : S1,S2 heard
RS : BAE on left side is decreased in isa,ma ,absent air entry on right side isa, iaa, ma
A -cardiogenic shock secondary to HFrEF with TYPE 1 Respiratory failure secondary to moderate hemorrhagic pleural effusion secondary to ?consolidation ,?malignancy with K/C/O CAD S/P PTCA ( 2 drug eluting stents )2 LCX 6 months back, AKI(pre renal ) with ischemic hepatitis
P-propped upto 30degrees
-Ryles tube feed- 50 ml milk 2 nd hrly
100 ml water 4 th hrly
- ryles tube suctioning before intake of food 2 nd hrly
-INJ PIPTAZ 4.5 mg/IV/ STAT
INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 10 ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 6 ml / hr
- INJ LASIX 5 AMP IN 30 ml ns at 4 ml / hr
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
- INJ LEVOFLOXACIN 500 mg IV / OD
- TAB ECOSPRIN - AV 75/20 mg rt/ hs
Soap notes :
Day 3 of admission :
S-Patient subjectively feeling better with complaints of cough
O -Temp : 98.7F
Bp : 90/70mmhg on 12 ml/hr dobutamine, 25ml/hr noradrenaline
Pr : 140bpm ,irregular, low volume
Rr:35 cpm
Spo2: 98% on 8 litres oxygen
CVS : S1,S2 heard
RS : BAE +,decreased breath sounds on right side
A -cardiogenic shock secondary to HFrEF with TYPE 1 Respiratory failure secondary to right massive pleural effusion secondary to consolidation with K/C/O CAD S/P PTCA ( 2 DES )6 months back ? Nosocomial
Pneumonia? pulmonary embolism
P-propped upto 30degrees
-INJ PIPTAZ 4.5 mg/IV/ STAT
INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 20 ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 12 ml / hr
- INJ LASIX 5 AMP IN 30 ml ns at 4 ml / hr
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
- NEB WITH IPRAVENT(6 th hrly) BUDECORT (12 th hrly)
-INJ PCM 650mg PO/ SOS
Soap notes :
Day 4 of admission :
ICU bed -3
Pt is C/C/C
Pedal edema persistent
S- C/O SOB on lying flat
O -Temp : 98.7
Bp : 90/70mmhg on 12ml/hr dobutamine, 22ml/hr noradrenaline
Pr : 111 bpm ,irregular, low volume
Rr:28 cpm
Spo2: 88% on RA in sitting, 96% on 12 lit oxygen
CVS : S1,S2 heard
RS : BAE + ,decreased breath sounds in, Rt infraaxiallary area, infrascapular areas
A -cardiogenic shock secondary to HFrEFwith EF 30% with TYPE 1 RESPIRATORY FAILURE (WITH NIV) secondary to consolidation with HAEMORRAHAGIC RT PLEURAL EFFUSION secondary to acute pulmonary embolism with contarst induced nephropathy with ischemic hepatitis with thrombus in rt atria and left atrial appendage ,ventricular apex,descending aorta
P- soft oral diet, oral fluids upto 1 lit
- O2 inhalation@4-6 lit/ min
-INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 22ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 10ml / hr
-INJ HEPARIN INFUSION 800 IU/hr 1.8 ml/ hr for 24 hrs
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
- NEB WITH IPRAVENT(6 th hrly) BUDECORT (12 th hrly)
-INJ PCM 650mg PO/ SOS
Soap notes :
Day 5 of admission :
ICU bed -3
Pt is C/C/C
Pedal edema persistent
S- C/O SOB on lying flat
O -Temp : 98.7
Bp : 90/70mmhg on 12ml/hr dobutamine, 22ml/hr noradrenaline
Pr : 111 bpm ,irregular, low volume
Rr:28 cpm
Spo2: 88% on RA in sitting, 96% on 12 lit oxygen
CVS : S1,S2 heard
RS : BAE + ,decreased breath sounds in, Rt infraaxiallary area, infrascapular areas
A -cardiogenic shock secondary to HFrEFwith EF 30% with TYPE 1 RESPIRATORY FAILURE (WITH NIV) secondary to consolidation with HAEMORRAHAGIC RT PLEURAL EFFUSION secondary to acute pulmonary embolism with contarst induced nephropathy with ischemic hepatitis with thrombus in rt atria and left atrial appendage ,ventricular apex,descending aorta
P- soft oral diet, oral fluids upto 1 lit
- O2 inhalation@4-6 lit/ min
INJ PIPTAZ 4.5 mg /IV/BD
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 22ml/ hr
- INJ DOBUTAMINE 250 MCG IN 50 ml NS at 12ml / hr
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
-INJ.ACETYLCYSTEINE 600 MG /IV/BD
TREATMENT GIVEN
Day1
- propped upto 30degrees
-Ryles tube feed- 50 ml milk 2 nd hrly
100 ml water 4 th hrly
- ryles tube suctioning before intake of food 2 nd hrly
-INJ PIPTAZ 4.5 mg/IV/ STAT
INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 10 ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 6 ml / hr
- INJ LASIX 5 AMP IN 30 ml ns at 4 ml / hr
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
- INJ LEVOFLOXACIN 500 mg IV / OD
- TAB ECOSPRIN - AV 75/20 mg rt/ hs
Day 2
propped upto 30degrees
-Ryles tube feed- 50 ml milk 2 nd hrly
100 ml water 4 th hrly
- ryles tube suctioning before intake of food 2 nd hrly
-INJ PIPTAZ 4.5 mg/IV/ STAT
INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 10 ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 6 ml / hr
- INJ LASIX 5 AMP IN 30 ml ns at 4 ml / hr
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
- INJ LEVOFLOXACIN 500 mg IV / OD
- TAB ECOSPRIN - AV 75/20 mg rt/ hs
Day 3
-propped upto 30degrees
-INJ PIPTAZ 4.5 mg/IV/ STAT
INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 20 ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 12 ml / hr
- INJ LASIX 5 AMP IN 30 ml ns at 4 ml / hr
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
- NEB WITH IPRAVENT(6 th hrly) BUDECORT (12 th hrly)
-INJ PCM 650mg PO/ SOS
Day-4
- soft oral diet, oral fluids upto 1 lit
- O2 inhalation@4-6 lit/ min
-INJ PIPTAZ 4.5 mg /IV/TID
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 22ml/ hr
- INJ DOBUTAMINE 2 AMP IN 50 ml NS at 10ml / hr
-INJ HEPARIN INFUSION 800 IU/hr 1.8 ml/ hr for 24 hrs
- INJ THIAMINE 100 mg IV/ TID in 100 ml ns
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
- NEB WITH IPRAVENT(6 th hrly) BUDECORT (12 th hrly)
-INJ PCM 650mg PO/ SOS
Day-5
soft oral diet, oral fluids upto 1 lit
- O2 inhalation@4-6 lit/ min
INJ PIPTAZ 4.5 mg /IV/BD
-INJ PANTOP 40mg /IV/ OD
- INJ NORAD- DS 22ml/ hr
- INJ DOBUTAMINE 250 MCG IN 50 ml NS at 12ml / hr
-TAB ECOSPRIN - AV 75/20 mg rt/ hs
-INJ.ACETYLCYSTEINE 600 MG /IV/BD
DEATH SUMMARY:
A 53 yr old cycle repaired by occupation presented to casuality With since 45 mins shortness of breath associated with cough with blood tinged sputum since 15 days , spo2 on presentation is 56%on room air , 64%on 15lit of o2, consentfor intubation was taken and was intubated , pulse, bp not recordable, carotid pulsations felt(112/min) and was started on vasopressors( noradrenaline, dobutamine) and was diagnosed to be in cardiogenic shock secondary to HFrEF with EF-30% with thrombus in right atria, LL atrial appendage, vent apex DEST aorta, CAD -S/P PTCA, DES TO LCX
Inj heparin infusion was started @1.8 ml/hr
Thoracocentesis was done in view hemorrhagic pleural effusion
Around 1:30 am on 12/9/21-bp , pulse not recordable, cpr was started according to ACLS guidelines. Despite the above resuscitation, treatment patient could not be revived and wqs declered dead on 12/9 /21@1:59 am
Immediate cause of death- sudden cardiac arrest secondary to cardiogenic shock
Antecedant cause of death : type 1 respiratory failure( with NIV) secondary to right consolidation with hemmorhagic right pleural effusion secondary to acute pulmonary embolism with ischemic hepatitis with thrombus in right atria, LL atrial appendage , vent apex , DEST aorta
CAD- S/P PTCA, DES TO LCX
















Comments
Post a Comment