5. Drug-induced edema
6. nutritional origin
ANEMIA - the kidney's function is to produce adequate amount of erythropoietin , when there is kidney damage these levels are reduced thereby causing anemia ( relative deficiency of erythropoeitin )
INDICATIONS OF IV SODIUM BICARBONATE :
- TO treat metabolic acidosis when the underlying disease is diarrhea, vomiting, or kidney-related diseases
- high blood potassium
- tricyclic anti-depressant overdose
- cocaine toxicity
CONTRAINDICATIONS :
- contraindicated in patients who are losing chloride
- it should be used with great care in patients of CCF, severe CKD due to its sodium content because in these conditions sodium retention is a problem
- it should be given in patients using corticosteroids with caution
USES OF ORAL SODIUM BICARBONATE ARE :
- as an antacid to treat heartburns, indigestion, upset stomach
WHY CONTRAINDICATED :
- Hypersensitivity
- metabolic/respiratory alkalosis and hypocalcemia - because alkalosis produces tetany
2. POTCHLOR syrup is given to correct hypokalemia
3. ORAL HYPOGLYCEMIC AGENTS - used as a diabetic agent to lower glucose levels in the blood
4. ANTI HYPERTENSIVES - to treat hypertension (to lower blood pressure value)
On day 2 :
1. Inj.HAI - used in type2 diabetes patients when their meat plan, weight loss, exercise, and antidiabetic drugs do not achieve targeted blood sugar levels
2. orofer - for treatment of iron and folic acid deficiency i.e anemia
3.PAN -Treatment of conditions due to excess acid secretion in the digestive system
4. LASIX - a diuretic which is used to reduce the risk of strokes, heart attacks, and kidney problems
contraindications are :
- kidney disease
- hypokalemia
- diabetes - when taken furosemide it is hard to control blood sugar levels
- liver disease
On day 3
1.tab Dytor - given to control fluid overload and blood pressure since the patient had higher blood pressure on day 3
2.telma - Telmisartan is given to treat hypertension, heart failure and diabetic kidney disease .may be because of its limitation that it reduces the amount of urine and increases kidney damage it could be stopped
3. Nicardia is given to lower blood pressure
4.Orofer and erythropoietin inj- in order to correct anemia and increase levels of erythropoietin which further corrects anemia
5. Shelcal - it is given to treat hypocalcemia
6. Potchlor syrup - to correct hypokalemia
7.nodosis - it is an antacid, to neutralize the excess acid present in the stomach
On day 4:
1. Lactulose - since the patient complained she had constipation she was given lactulose after which she passed the stools
2.inj.monocef- it is an antibiotic. Used to treat UTI or any other infections
3. Protein x powder - given since the patient is malnourished
but excess use can cause coma, hepatic damage, metabolic disturbances, unpleasant taste in the mouth
On day 5
The patient was further evaluated to improve her condition
what was the indication for dialyzing her and what was the crucial factor that led to the decision to dialyze her on the 3rd day of admission?
- severe breathlessness due to pulmonary edema
- acid-base problems ( METABOLIC ACIDOSIS )
- pericarditis
- electrolyte imbalance
On 3rd day of her admission, the crucial factor that led to the decision to dialyze her was due to - FLUID OVERLOAD / PULMONARY EDEMA REFRACTORY TO DIURETICS and Refractory anuria
what are the other factors other than diabetes and hypertension that led to her current condition?
it may be due to anemia, vascular disease, and constipation
what are the expected outcomes in this patient? Compare the outcomes of similar patients globally and share your summary with reference links?
as mentioned in the above link :
chronic pressure overload, progressive volume overload, cardiomyopathy with the additional risk factor of Diabetes, Anemia could lead to preserved LVEF / reduced LVEF which further lead to the outcome of :
- Progression of CKD
- HF hospitalization
- Sudden arrhythmic death
- Pump failure of death
How and when would you evaluate her further for cardio-renal HFpEF and what are the mechanisms of HFpEF in diabetic renal failure patients?
Evaluation for HFpEF must be done on the day of admission itself if there is suspicion of heart-related disorder such as heart failure as per the patient's symptoms, clinical examination, and laboratory diagnosis
Evaluation for cardio-renal HEpEF :
- Echocardiography - provides information on chamber volumes, ventricular systolic and diastolic dysfunction, wall thickness, valve function, and filling pressures
- Chest radiography - to screen for other sources of dyspnea
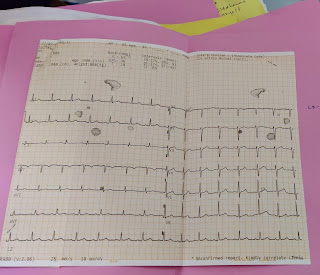
- Electrocardiography - to detect rhythm disturbances or evidence of prior myocardial damage or pericardial disease
- MRI
- global longitudinal strain analysis
- whole -body bioimpedance technique
- extended cardiac rhythm monitoring
Emerging diagnostic options include :
- Pulmonary artery ambulatory monitoring
- thoracic impedance monitoring
decreased renal blood flow leads to the stimulation of the RAAS mechanism resulting in :
- sodium, water retention leading to volume overload thereby increasing blood pressure and cardiac work, myocardial fibrosis finally causing heart failure
- leads to vasoconstriction leading to increased afterload, increased blood pressure, leading to heart failure
What are the efficacies over placebo for the available therapeutic options being provided to her for her anemia?
referred link as follows
https://pubmed.ncbi.nlm.nih.gov/19245362/
https://clinicaltrials.gov/ct2/show/NCT01114139
What is the utility of tools like the CKD-AQ that assess the frequency, severity, and impact on daily activities of symptoms of anemia of CKD? Is Telegu among the 68 languages in which it is translated?
CKD-AQ - about frequency, severity of symptoms, signs associated with anemia.
https://academic.oup.com/ckj/advance-article/doi/10.1093/ckj/sfz091/554348
https://www.smartpatients.com/trials/NCT034091072
what is the contribution of PEM to her severe hypoalbuminemia? what is the utility of tools such as SGA( subjective global assessment ) in the evaluation of malnutrition in CRF patients
Nutritional deficiencies particularly that of iron and zinc and decreased supply of amino acids to the liver causes reduced production of albumin levels thus leading to hypoalbuminemia
Nutritional status as determined by Subjective Global Assessment -Dialysis Malnutrition Score is a useful and reliable index for identifying patients at risk for malnutrition and it correlates well with the anthropometric and biochemical assessment. May be integrated into the regular assessment of malnutrition in patients on maintenance hemodialysis
Differences in the diagnosis of a 45-year-old female and a 58-year-old man ;
As per the clinical findings of the patient of 45-year-old
- Albuminuria
- decreased urine output
- Abnormal renal biopsy
- on USG - loss of CMD and increased echogenicity
- Hence could be diagnosed as CKD due to diabetic nephropathy
As per 58-year-old male patient:
- Increased bun/serum creatinine >20:1 which may indicate AKI
- Low urinary output
- Flank pain
- On USG - there's no increase in echogenicity and other abnormality is not detected and left kidney size reduced
- Hence could be diagnosed as AKI
Differences in management:
45-year-old patient :
- Potchlor was given to correct hypokalemia
- shelcal for hypocalcemia
- Lasix to correct fluid overload
- anti-diabetic and antihypertensive agents are given
- further investigations are done to improve the patient condition
58-year-old patient :
- Piptaz - an antibiotic
- Amlong tablet - for treatment of hypertension
- Lasix to combat fluid overload
- Pantop - an antacid
- HAI - to reduce blood sugar levels
Differences in outcomes
in AKI :
In CKD :
Would you agree with the provisional diagnosis of a 58-year male patient as per the online case report?
Yes I would agree with the provisional diagnosis that is AKI since the patient has bun/creatinine ratios increased >20:1 and he complained of burning micturition, hyponatremia (mild)
References :
1.Dr.Alekya Reddy mam's blog
2. Dr.Bhavya mam's blog
3.Harrison's book of medicine
4.all the links shared at their respective texts




Comments