A 20yrs old male patient
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Unit 1 admission
A 20 yrs old male patient daily laborer by occupation came to casuality with cheif complaints fever since yesterday , head ache since yesterday
Patient was apparently asymptomatic yesterday, came with cheif complaints of fever around yesterday night, high grade fever associated with chill and rigor on , off relieved on medication , no history of cold, cough.
History of head ache since yesterday , pain in frontal region, throbbing type of pain , during episodes of fever, photophobia + and phonophobia + aggrevating with position variation, lacrimation(-), diplopia(-).
No history of nausea, vomiting, loose stools
No history of chest pain, palpitation, syncopal attacks
No history of sob, orthopnea, palpitation
No history of pedal edema, facial puffiness
No history of burning micturition
Past history:
No history of similar complaints in past
Not a known case of dm, htn, tb, asthma , epilepsy
No history of previous surgeries and no history of previous blood transfusions
Personal history:
Diet: mixed
Appetite: normal
Bowel, bladder habits : normal, regular
Not a smoker, alcoholic
Vitals :
Patient was C/C/C
PR : 84BPM.
RR : 18 CPM
BP : 90/60 mm of Hg.
Spo2 : 99 % at RA.
GRBS : 99 mg/dl
On Examination :
Patient is thin built and malnourished.
No pallor
No icterus, cyanosis, lymphadenopathy, Clubbing, pedal edema
Systemic Examination :
CVS: S1, S2 heard, No murmurs.
RS: Position of trachea : Central
BAE : +
NVBS Heard.
P/A : Soft, Non Tender, No palpable masses or swelling.
CNS : NAD.
Diagnosis: dengue
On 15/8/2021
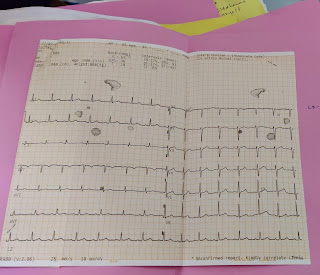
Ecg
















Comments
Post a Comment