A 15 yrs boy with bleeding gums
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
Unit 1 admission:
15 year old boy came to the OPD with the chief complaints of
Bleeding gums since 3 days
Oral ulcers since 3 days
Blackish discoloration on RT side of abdomen since 4 days
HOPl:
Pt was apparently asymptomatic 4 days back,when the mother noticed blackish blue discoloration on the right iliac area ,with no alleged history of trauma , no tenderness
Followed by bleeding gums and oral ulcerations with low grade of fever since 3 days
No H/O cough,cold,pain abdomen,loose stools, vomitings.
- H/O blackish hyperpigmented spots on abdomen and dorsum of forearm.
- no similar complaints in the past
-No H/O delayed milestones.
- pt is active in school
On examination:
Pt is conscious, coherent and cooperative
Pallor - present
Moderate dehydration
Vitals:
Afebrile
PR: 80
BP: 80/50mmhg
Spo2: 96%
CVS: s1,S2 heard
RS: BAE +, NVBS.
P/A: soft ,non tender
BS+
CNS: Normal
Blackish blue discoloration over right iliac region, inner aspect of thigh
Investigations:
Chest xray
Hb:8.7
TLC:2,500
PLT:11,000
PCV-: 25.7
MCHC: 33.9
MCV: 75.1
RBC count: 3.42
LFT:
TB: 1.29
DB: 0.31
AST: 21
ALT: 18
ALP: 198
TP: 6.3
Alb: 3.7
A/G: 1.45
NS1 antigen - negative
diagnosis:
Fever with pancytopenia ( ? Aleukemic leukemia) with cervical lymphedenopathy with splenomegaly
INVESTIGATIONS
ON 21/9/21
Hemogram
Hb- 7.4
Tlc-2,100
Rbc- 2.73
Plt-30,000
Serum iron- 69
Pt- 16 sec
Inr-1.11
Aptt-33 sec
Serum LDH- 294
recticulocyte count-0.3%
Stool for occult blood is negative
Hemogram on 22/9/21
Hb- 6.7
Tlc - 1600
Plt- 9,800
Rbc - 2.65
Pcv- 20.5
Treatment given :
Day 1
1) intravenous fluids( RL, NS, DNS)
2) INJ PANTOP 20 mg IV/ OD 8 am
3) INJ CEFTRIAXONE 1 gm IV/ BD
4) Tab DOLO 500 mg 1/2 tab (sos)
5) ZYTEE GEL FOR L/A
6) Tab DOXY 100mg PO/ OD
Day 2
1) intravenous fluids( RL, NS, DNS)
2) INJ PANTOP 20 mg IV/ OD 8 am
3) INJ CEFTRIAXONE 1 gm IV/ BD
4) Tab DOLO 500 mg 1/2 tab (sos)
5) ZYTEE GEL FOR L/A
6) Tab DOXY 100mg PO/ BD
Discharge summary:
Date-22/9/21
Ward- icu
Unit- gm1
Dr valli( intern)
Dr akshitha( intern)
Dr tejaswini( intern)
Dr roshna( intern)
Dr kusuma( intern)
Dr raveen( pgy1)
Dr k vaishnavi( pgy3)
Dr nikhitha( pgy3)
Dr hareen( sr)
Dr arjun( ap)
Dr rakesh biswas( hod)
Diagnosis: fever with pancytopenia(? Aleukemic leukemia - pt requires bone marrow aspiration
Cervical lymphedenoapthy with splenomegaly
Clinical history , findings
15 year old boy came to the OPD with the chief complaints of
Bleeding gums since 3 days
Oral ulcers since 3 days
Blackish discoloration on RT side of abdomen since 4 days
HOPl:
Pt was apparently asymptomatic 4 days back,when the mother noticed blackish blue discoloration on the right iliac area ,with no alleged history of trauma , no tenderness
Followed by bleeding gums and oral ulcerations with low grade of fever since 3 days
No H/O cough,cold,pain abdomen,loose stools, vomitings.
- H/O blackish hyperpigmented spots on abdomen and dorsum of forearm.
- no similar complaints in the past
-No H/O delayed milestones.
- pt is active in school
On examination:
Pt is conscious, coherent and cooperative
Pallor - present
Moderate dehydration
Vitals:
Afebrile
PR: 80
BP: 80/50mmhg
Spo2: 96%
CVS: s1,S2 heard
RS: BAE +, NVBS.
P/A: soft ,non tender
BS+
CNS: Normal
Investigations:
Hemogram ( 20/9/21)
Hb:8.7
TLC:2,500
PLT:11,000
PCV-: 25.7
MCHC: 33.9
MCV: 75.1
RBC count: 3.42
LFT:
TB: 1.29
DB: 0.31
AST: 21
ALT: 18
ALP: 198
TP: 6.3
Alb: 3.7
A/G: 1.45
NS1 antigen - negative
Serology - negative
ON 21/9/21
Hemogram
Hb- 7.4
Tlc-2,100
Rbc- 2.73
Plt-30,000
Serum iron- 69
Pt- 16 sec
Inr-1.11
Aptt-33 sec
Serum LDH- 294
recticulocyte count-0.3%
Stool for occult blood is negative
Hemogram on 22/9/21
Hb- 6.7
Tlc - 1600
Plt- 9,800
Rbc - 2.65
Pcv- 20.5
Chest x ray - normal
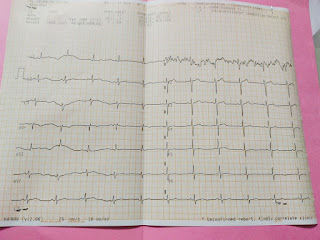
Ecg- normal
Usg abdomen- mild ascites, splenomegaly
Usg neck - bilateral cervical lymphedenopathy
Treatment given:
Day 1
1) intravenous fluids( RL, NS, DNS)
2) INJ PANTOP 20 mg IV/ OD 8 am
3) INJ CEFTRIAXONE 1 gm IV/ BD
4) Tab DOLO 500 mg 1/2 tab (sos)
5) ZYTEE GEL FOR L/A
6) Tab DOXY 100mg PO/ OD
Day 2
1) intravenous fluids( RL, NS, DNS)
2) INJ PANTOP 20 mg IV/ OD 8 am
3) INJ CEFTRIAXONE 1 gm IV/ BD
4) Tab DOLO 500 mg 1/2 tab (sos)
5) ZYTEE GEL FOR L/A
6) Tab DOXY 100mg PO/ BD
Refer to higher centre in view of bone marrow biopsy, suspicion of malignancy







Comments
Post a Comment