A 25 yr old male with sob
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
UNIT 1 ADMISSION
Dr k vaishnavi( pgy3)
Dr nikhitha( pgy3)
Dr raveen( pgy1)
ICU BED 4
A 25 yr old male , factor worker came to casuality with complaints of fever since 3 days , vomitings since 2 days ,loose sto
ols since today, cough since 2 days, grade 4 sob since evening, chest pain , lower back pain, abdominal pain since evening
Pt was apparently asymptomatic 3 days ago then he devwloped high grade fever, continuous, associated with chills and rigor
Vomitings since 2 days 4 to 5 episodes water in consistency, non blood tinged associated with nausea occurs immediately after food intake
Cough since 2 days with scanty sputum white color
Loose stools since today 3 episodes ,watery in consistency associated with diffuse pain abdomen
No history of decreased urine output, burning micturition, chest pain , lower back pain since evening
Grade 4 sob since evening( 8 pm)
No h/ o orthopnea, pnd, pedal edema
Past history:
Not ak/c/o hypertension, diabetes mellitus, tuberculosis, asthma, coronary artery disease
Not received covid vaccination
Personal history:
He is not married, factory worker by occupation, with mixed diet , normal appetite,
regular bowel, bladder habits non alcoholic , non smoker
Family history : not significant
General examination:
Pt c/ c/ c
Vitals:
Bp- 100/60mmhg
Pr-184 bpm regular
Rr-46cpm
Temperature-105 degress
Spo2- 94-96% on ra.
Ecg monitor showing Psvt.
Immediately carotid sinus massage was done .
1) INJ NEOMAL 1G IV STAT
2) INJ TRAMADOL 1 AMP in 100 ML NS IV given as pt was complaining of low back ache and generalised body aches
3) COLD ICE PACKS WERE PLACED.
4)IVF 3 unitd NS bolus given.
5) INJ CEFTRIAXONE 1 G IV BD.
After 10 min rate reduced and rythm was normal.
BP-80/60 mmhg
PR - 120 bpm ,regular.
Rr-40/min.
ABG showing
PH- 7.419
Pco2- 24.2
Po2- 92.2
Spo2- 93.6
Hco3- 15.4
Pt is on norad 6 ml/ hr
Systemic examination
Cvs- s1, s2 heard
Rs- bAE+, NVBS
P/A - soft , tendernesa in right hypochondriac region
Cns- intact
Provisional diagnosis :psvt
Pancytopenia under evaluation, fever under evaluation- ? Acute gastroenteritis(typhoid fever/? leptospira/ ? Viral pyrexia ? Pre renal AKI
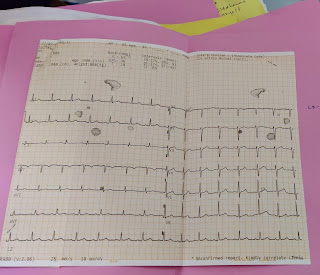
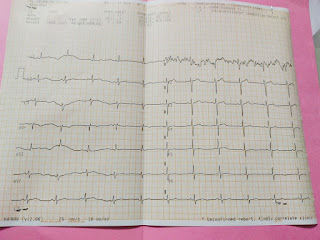
ECG at the time of admission
Investigations on 27/9/21
Hemogram:
Hb- 8.9
Tlc- 2,100
Plt- 37,000
Rbc- 3.82
Pcv- 26
Mcv- 68.1
Mch- 23.3
Mchc- 34.2
Serum urea- 89
Serum creatinine- 2.1
Na+ 128
K+ 3
Cl- 101
Lft
Tb-0.89
Db-0.17
Ast- 34
Alt- 26
Alp- 110
Alb- 2.29
A/G- 1.34
Serology -negative
Rapid dengue- negative
Hemogram on 27/09/21 mrng sample
Hb- 8.9
Tlc- 3,500
Rbc- 3.82
Plt- 65000
Esr-80
Recticulocyte count- 0.5
Serum k+ 4.5
Serum electrolytes
Na+ 128
Cl- 101
Serum mg+2 1.8
Serum urea- 89
Serum creatinine- 2.1
Serum LDH- 365
On 28/09/21
Hb- 10.6
Tlc- 7,100
Plt- 66,000
Rbc- 4.55
Serum urea- 65
Serum creatinine- 1.6
Na+ 132
K+ 3.9
Cl- 102
On 29/09/21
Hb- 10.8
Tlc-7,400
Rbc- 4.68
Plt- 80,000
Soap notes
Icu bed- 4
Day 3
S- Patient is comfortably sleeping on his bed. He says his dyspnea and cough have reduced comparatively.
O-
pt is c/c/c
Vitals:
Bp- 100/70 mmhg
Pr- 91 bpm regular , normal volume
Temperature- 99.6F
Grbs- 109mg
I/0-2100/1400
cvs- s1,s2 + no murmur
Rs- nvbs+ wheeze in ISA
P/A- soft , tenderness in rt hypochondriac, bs+
A- HFr EF with EF- 35% secondary to severe PAH( RVSP=68 mmhg) ? Viral myocarditis with pancytopenia under evaluation secondaey to ? Typhoid ? Viral with pre renal AKI
P-
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ NORAD- DS@5ml/ hr
8) T. PCM 650 mg/ po/ TID
9) INJ ZOFER 4mg / IV /BD
10) INJ NEOMOL100 ml/ IV/ SOS
11) T .ULTRACET PO/ SOS
12) T ATORVAS 20 mg po/ hs
13) monitor vitals temp, bp hrly
14) strict I/0 charting
15 ) GRBS- 12 th hrly
Soap notes
Icu bed- 3
Day 4
S- Patient is comfortably sleeping on his bed. He says no dysnea, no cough decreased pain abdomen
O-
pt is c/c/c
Vitals:
Bp- 100/80 mmhg @ 1ml / hr norad
Pr- 88 bpm regular , normal volume
Temperature- 98.6F
Grbs- 99mg
I/o -900/1500
cvs- s1,s2 + no murmur
Rs- bae+ nvbs+
P/A- soft , bs+
A- HFr EF with EF- 35% secondary to severe PAH( RVSP=68 mmhg) ? Viral myocarditis with pancytopenia under evaluation secondaey to ? Typhoid ? Viral with pre renal AKI
P-
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ NORAD- DS@1ml/ hr
8) INJ ZOFER 4mg / IV /BD
9) T .ULTRACET PO/ SOS
10) T.PCM 650 mg PO/ SOS
12) monitor vitals temp, bp hrly
13) strict I/0 charting
14 ) GRBS- 12 th hrly
Soap notes
Ward case
Day 5
S- Patient is comfortably sleeping on his bed. He says no dysnea, no cough decreased pain abdomen
O-
pt is c/c/c
Vitals:
Bp- 110/70 mmhg
Pr- 76 bpm regular , normal volume
Temperature- 98.6 F
cvs- s1,s2 + no murmur
Rs- bae+ nvbs+
P/A- soft , bs+
A- cardiogenic shock ( resolved)
HFr EF with EF - 46% severe PAH secondary to ? Viral myocarditis/ ? Typhoid fever
Pancytopenia secondary to infectious etiology
Pre renal AKI
PSVT - resolved
P-
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ ZOFER 4mg / IV /BD
8)T.PCM 650 mg PO/ SOS
9)INJ PAN 40 mg IV/ OD
10) monitor vitals temp, bp hrly
Treatment given
Day 1
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ NORAD- DS@5ml/ hr
8) T. PCM 650 mg/ po/ TID
9) INJ ZOFER 4mg / IV /BD
10) INJ NEOMOL100 ml/ IV/ SOS
11) T .ULTRACET PO/ SOS
12) T ATORVAS 20 mg po/ hs
13) monitor vitals temp, bp hrly
14) strict I/0 charting
15 ) GRBS- 12 th hrly
Day 2
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ NORAD- DS@5ml/ hr
8) T. PCM 650 mg/ po/ TID
9) INJ ZOFER 4mg / IV /BD
10) INJ NEOMOL100 ml/ IV/ SOS
11) T .ULTRACET PO/ SOS
12) T ATORVAS 20 mg po/ hs
13) monitor vitals temp, bp hrly
14) strict I/0 charting
15 ) GRBS- 12 th hrly
Day 3
1) Fluid restriction < 1.5 l/ day
2) Salt restriction< 2.5 gm / day
3) INJ LASIX 20 mg / IV/ BD
4) INJ MONOCEF 1gm / IV/ BD
5) T. DOXY 100 PO/ / BD
6) INJ OPTINEURON 1amp in 100 ml/ NS IV/ OD
7)INJ ZOFER 4mg / IV /BD
8)T.PCM 650 mg PO/ SOS
9)INJ PAN 40 mg IV/ OD
10) monitor vitals temp, bp hrly







Comments
Post a Comment