A 45 YR OLD FEMALE WITH FEVER
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
UNIT 1 ADMISSION
A 45 yr old female pt came with cheif complaints of fever with chills since 3 days
Hopi - pt was apparently asymptomatic 3days back then she developed high grade fever associated with chills ,rigors
No c/o of cough, cold,
No c/o of chestpain , palpitations,syncopal attacks
No c/o of sob , orthopnea ,pd
Nause present , no vomitigs,loose stools
No c/o of abd distention
C/o of , burning micturition, decreased urine output
No h/o HTN,, CVA, CAD,TB, epilepsy.
K/c/o dm since 2 yrs on regular medication
Personal history:
Decreased appetite
Bowel and bladder movements are regular
Non alcoholic , non smoker
The patient is conscious coherent and cooperative
Moderately built and moderately nourished.
Vitals:
PR:80bpm
BP:110/80 mmHg
RR:16cpm
Spo2:99% at RA
GRBS: 560mg%
P/A:
Shape of abdomen: scaphoid
Abdominal tenderness is present in epigastric region
Hernial orifices- normal
No free fluid
Liver and spleen - not palpable
Bowel sounds are present
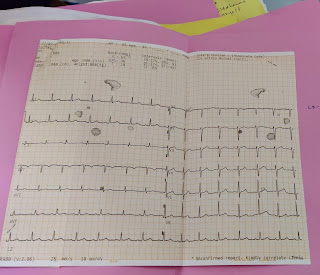
CVS: s1 ,s2 heard
RS: vesicular breath sounds are heard
CNS: normal
Provisional diagnosis:
Viral pyrexia with thrombocytopenia ( Dengue)
INVESTIGATIONS:
Hemogram on 30/9/21
HB-14.7gm/dl
TLC- 5,600cells/cu.mm
RBC-5.67 million/cu.mm
PLT-40,000 lakhs/cu.mm
CUE:
Serum urea-43 mg/dl
Serum creatinine- 1.2 mg/dl
Serum electrolytes:
Na+: 134 meq/l
K+: 4.5 meq/l
Cl-: 96 meq/l
LFT
TB-0.93 mg/dl
DB-0.2 mg/dl
AST-107units/l
ALT-81 units/l
ALP-208 units/l
ALB-3.3gm /l
MALARIAN PARASITE - NEGATIVE
BLOOD GROUP- O POSITVE
NS1 ANTIGEN- POSITIVE( DENGUE)
CHEST XRAY
ON 31/8/21
HB-13.4gm/l
TLC-6.700cells/cu.mm
RBC- 4.67million/cu.mm
PLT-45,000lakhs/cu.mm
FBS-357mg/dl PLBS-324mg/dl
HBA1C- 78mg/dl
ON 1/9/21
HB-14.1gm/dl
TLC-9,600cells/cu.mm
RBC-4.96 million/cu.mm
PLT-35,000lakhs/cu.mm
ON 2/9/21
HB-12.8 gm/dl
TLC-6,800cells/cu.mm
RBC-4.48millions/cu.mm
PLT-70,000lakhs/cu.mm
ON 3/9/21
HB-13.1 gm/ dl
TLC-5,700 cells/ cu.mm
RBC- 4.60 millions/cu.mm
PLT- 80,000 lakhs/cu.mm
ON 4/9/21
HB-12.8 gm /dl
TLC-6,300cells/cu.mm
RBC-4.54 millions / cu.mm
PLT-1. 2 lakhs/cu.mm
TREATMENT GIVEN
Day-1
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
Day-2
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
Day-3
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
Day-4
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
Day-5
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
DISCHARGE SUMMARY:
patient came to casuality with following history
Following examination was done
UNIT 1 ADMISSION
Dr. Aashitha
Dr. Vinay
A 45 yr old female pt came with cheif complaints of fever with chills since 3 days
Hopi - pt was apparently asymptomatic 3days back then she developed high grade fever associated with chills ,rigors
No c/o of cough, cold,
No c/o of chestpain , palpitations,syncopal attacks
No c/o of sob , orthopnea ,pd
Nause present , no vomitings,loose stools
No c/o of abd distention
C/o of , burning micturition, decreased urine output
No h/o HTN,, CVA, CAD,TB, epilepsy.
K/c/o dm since 2 yrs on regular medication
Personal history:
Decreased appetite
Bowel and bladder movements are regular
Non alcoholic , non smoker
The patient is conscious coherent and cooperative
Moderately built and moderately nourished.
Vitals:
PR:80bpm
BP:110/80 mmHg
RR:16cpm
Spo2:99% at RA
GRBS: 560mg%
P/A:
Shape of abdomen: scaphoid
Abdominal tenderness is present in epigastric region
Hernial orifices- normal
No free fluid
Liver and spleen - not palpable
Bowel sounds are present
CVS: s1 ,s2 heard
RS: vesicular breath sounds are heard
CNS: normal
Provisional diagnosis:
Viral pyrexia with thrombocytopenia (? Dengue)
On giving following treatment
1)plenty of oral fluids
2) intravenous fluids(normal saline, ringer lactate 100ml/hr)
3) Inj PANTOP 40 mg IV/ BD
4)Inj ZOFER 4mg IV/ TID
5) Inj HUMAN ACTRAPID INSULINS/C
8am- 1pm -8pm
6) vitals monitoring
Patient platelet count gradually increased
On 30/8/21
PLT-40,000 lakhs/cu.mm
On 31/8/21
PLT-45,000lakhs/cu.mm
On 1/9/21
PLT-35,000lakhs/cu.mm
On 2/9/21
PLT-70,000lakhs/cu.mm
On 3/9/21
PLT- 80,000Lakhs/cu.mm
On 4/9/21
PLT-1.2 lakhs/cu.mm
As the platelet count increased and symptoms subsided she was planned to discharge on 4 /9/21





Comments
Post a Comment